Brain tumors
Primitive intracranial tumors are relatively uncommon: about 10 cases per 100,000 inhabitants per year. Most of them originate from nutritional and supporting tissue (gliomas), from the meninges (meningiomas), and from the myelin sheath of the cranial nerves (neuromas). The brain tumor does not metastasize, except in rare cases.
The ” benignity” of some intracranial tumors does not always correspond to the possibility of healing. In fact, in some locations, even partial removal of the tumor can be very risky for the non-negligible mortality (as in the case of lesions adjacent to or growing into the brain stem), or the possible morbidity, as in the case of tumors that arise in the vicinity of “eloquent” brain areas, (expressing a particular function, such as language or movement) of the cranial nerves (optic, oculomotor, trigeminal, facial, acoustic, vagus, etc.) or encasing large arteries and veins.
The main objective of the modern Neurosurgical oncology consists of the maximal removal of the tumor with minimization of complications.
Various tools have improved the performances in the surgical removal of brain tumors in recent years :
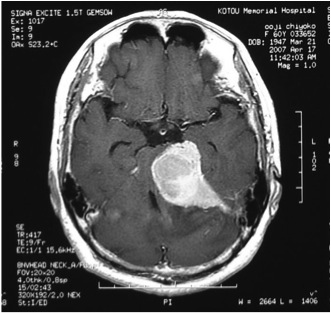
A. acquisition and processing of images both pre- and intraoperative (thin-slice CT, MRI, functional MRI and tractography, navigational systems, 2D and 3D endoscopy, ultrasounds)
B. increasingly sophisticated surgical equipment (microscope integrated with navigator, fine bipolar forceps, microsurgical instruments dedicated for each procedure, ultrasonic aspirators, lasers).
Among these instruments essential for the successful of the procedure, an increasingly important place is occupied today by the flexible hand-held fiber laser.
Recently, the possibility of using the CO2 and Thulium Lasers with hand-held flexible fibers (directly used by the surgeon) has relaunched the use of Laser in Neurosurgery. On the basis of the first international experience we started to use the CO2 Laser and Thulium Laser in the procedures for removal of selected intracranial tumors, both for “cutting”, coagulating, and “vaporizing” the mass, observing some peculiarities and evaluating its effectiveness and safety.
Adopting the necessary technical-surgical procedures and the right indications, the flexible CO2 Laser and Thulium Laser give a valuable aid in the microsurgical removal of intracranial tumors, especially meningiomas, allowing you to cut the tumor capsule, to coagulate pathological newly formed microvessels and to vaporize the mass (debulking) and removing the dural attachement of meningioma too.
The CO2 Laser is very useful for cutting hard tumors (such as fibrous meningiomas) and allows to do high-risk maneuvers in complete safety: this is due to its natural strong water absorption due to the wavelength of 2 um.
On the other hand, Thulium Laser proved to be very effective in the surgical removal of Meningiomas and Neuromas, especially if highly vascularized.
At the end of December 2013, our team has operated on over 80 intracranial tumors, by using CO2 and Thulium Lasers, 52 of which were meningiomas (2/3 supratentorial and 1/3 in the posterior cranial fossa). Total excision was possible in 27 meningiomas, subtotal in another 21 (with small residuals in areas at risk, in order to avoid significant neurological deficits) and partial in 2 giant meningiomas in elderly patients. In the relationship cut/coagulation/vaporization the percentage has averaged 55/28/17 for extra-axial tumors (meningiomas and neuromas), compared to the 15/65/20 percentage in other tumors. This is justified by the fibrous and more compact nature of meningiomas and their vascularization which makes it more difficult to remove by using traditional tools.
The CO2 Laser has been proven very safe and useful in the debulking and in the cutting and vaporization of dural attachment of meningiomas and in the removal of low-consistency neuromas, especially at the level of the skull base.
The Thulium Laser resulted effective, precise, and safe expecially in the surgical removal of high vascularized tumors (skull base meningiomas, fibrous acoustic neuromas).
References :
Attachments :




