Batson’s epidural venous plexus
Article written by : Raffaele Roperto
What is meant by the term lumbar spinal stenosis?
The term “lumbar spinal stenosis” refers to a narrowing of the spinal canal, the root canal and/or intervertebral foramina, from which emerge the nerve roots, which causes the compression of one or more nerve roots.
Conditions, congenital or acquired, which cause narrowing of the diameter of the lumbar vertebral canal realize a mismatch between containing structures and contained structures, from which arise those painful and/or deficit symptoms.
Are there risk factors and/or more susceptible categories?
In acquired stenosis (the most common), the predominant factor is age. The peculiarities of degenerative changes (arthritic), that is related to the “natural aging of bone and ligamentous structures”, typical of the lumbar rachis were extensively studied by two Authors, who deserves credit for having. The first, William Kyrkaldy Willis, highlighted the progressive disappearance of the anatomical and functional characteristics of the lumbar spine (the pathophysiology of spinal degeneration), which since then goes under the name of “DEGENERATIVE CASCADE”. The second, Henk Verbiest, firstly described the foraminal stenosis (1940) and related symptoms, which were gathered in a syndrome known as S. of Verbiest.
How can you orient yourself to understand what you have is more than just a backache?
Characteristic symptom of lumbar spinal canal stenosis, called Pseudo-claudicatio Spinalis is the pain radiating to the lower limbs after the subject has started deambulation, that forces the subject to stop and find relief. The name (Claudicatio) is borrowed from a similar symptom caused by a shortage of spraying blood in the lower limbs in cases of diseases of the arteries, which carry blood to the lower limbs. In these cases, where the demand for oxygen by the muscles is increased (increased muscle activity as it happens in the course of walking), and the blood supply is deficient, the lack of oxygen available for the muscle activity is expressed on a clinical level with painful symptoms, which fades only when such request fails (and the subject stops his muscular activity).
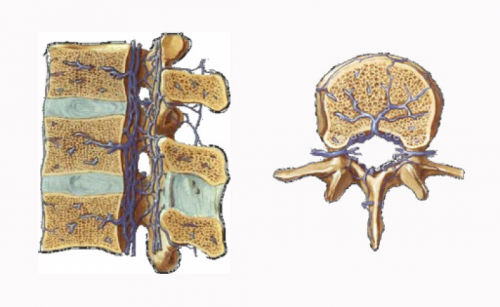
§If the clinical picture is similar (and from this derives the similar name) the pathogenesis of the pain is quite different. The necessary increase in arterial blood flow to the muscle groups of the lower limbs leads, of course, to an increase in the flow of venous blood from the district of the lower limbs. This leads to a sort of “traffic jam” of the effluent venous circulation , and consequently to a use of all other venous circles available; among them the Batson’s epidural venous plexus (Fig. 1). This network of venous vessels present in the vertebral canal and placed all around the dural sac, swells by increasing the diameter of its vessels. In a condition of the already existing vertebral canal stenosis such a change can only worsen the conflict between container and content, and consequently the clinical symptoms.
How to get to a diagnosis?
The diagnosis of stenosis of the lumbar vertebral canal is essentially clinical, therefore it is essential a neurosurgical examination. To confirm the clinical diagnosis are necessary instrumental diagnostic investigations :
X Ray L/S
Dynamic X Ray L/S Axially loaded.
Thin slice CT multiplanar reconstructions , and in selected cases an Axial load CT (Axially loaded CT L/S)
MRI L/S confirms the reduction of the channel amplitude indicating involvement of several vertebrae in the sagittal scans and shows the narrowing of the dural sac and the roots bundling . An electromyography (EMG) will confirm the radicular suffering and its exact levels.
Treatment, which and when!
The first time, depending on the degree of stenosis, the Restorative Treatment must be provided (non-surgical):
NSAIDs
Prolonged bed rest
Epidural steroid injections
Calcitonin
Magnet therapy, iontophoresis
Surgeon Treatment:
The aim of surgical treatment of lumbar spinal stenosis is the decompression of neural structures (spinal roots). In order to achieve this goal, the posterior surgical aggression is necessary and removal (targeted and never too large) of the structures (laminae, zygapophyses, yellow ligaments, joint capsules) responsible – for their hypertrophy or congenital alteration – of compression. It is always necessary to remember that the removal of the anatomical structures of the Motion Segment (this term refers to the two neighboring vertebrae, with all the disc and ligaments binding them together) may lead to an excess of intervertebral movements (instability) and then to a new pathological situation. In some cases, in relation to the presence of the vertebral “instability” diagnosed with radiographic examinations in flexion-extension and / or with CT, it can bind to surgical decompression and vertebral stabilization by screw fixation and arthrodesis. The choice of treatment is undertaken, both to restore stability to a portion of the column that has lost (because of degenerative arthritic alterations) the properties and limits of physiological movement, both to prevent the onset of pathological motility, linked to the necessary decompression of the nervous structures.
References :
Attachments :




